Episode 37 - Finding Hope After Miscarriage: Practical Fertility Support with Alison Hall
Healthily | 05/13/25
In this episode of Healthily, Nicola speaks with fertility-focused nutritional therapist Alison Hall to explore the sensitive and emotional topic of fertility after miscarriage. With empathy and expertise, Alison shares a wealth of practical, empowering insights—ranging from nutrition and lifestyle guidance to the often-overlooked role of thyroid health. Whether you've experienced loss, are supporting someone who has, or want to better understand fertility, this episode offers tools, tests to consider, and—most importantly—a message of hope and ownership.
TAKEAWAYs
✔️ Big-Picture Philosophy: From “Infertility” to “Subfertility” & Root-Cause Exploration
The guest prefers the term “subfertility” over “infertility,” because “infertility” often feels like a fixed, hopeless label — whereas “subfertility” allows room for investigation, nuance, and multiple contributing factors.
Rather than treating fertility as a single problem (e.g. “no egg,” “low sperm,” “polycystic ovary”), the approach is comprehensive: look at the whole picture — lifestyle, medical history, environment, emotional health, gut and reproductive microbiomes, nutrition, stress, toxins.
The belief: in most cases, there is a reason things aren’t working optimally — even if conventional testing hasn’t found it yet. The job of a thorough practitioner is to uncover those underlying causes.
✔️ Why Conventional Treatments/Labels Are Often Insufficient
Many fertility issues are filed under “unknown” or “unexplained infertility” because standard diagnostics rarely dig deep enough. This can leave couples feeling powerless and resigned.
Common medical pathways may ignore factors like immune function, microbiome balance, environmental toxin exposure, subtle nutrient deficiencies, or even male partner’s health — all of which can affect fertility outcomes.
Emotional burden and loss (e.g. miscarriage) are often framed as “just part of the risk,” without deeper exploration of what may have contributed.
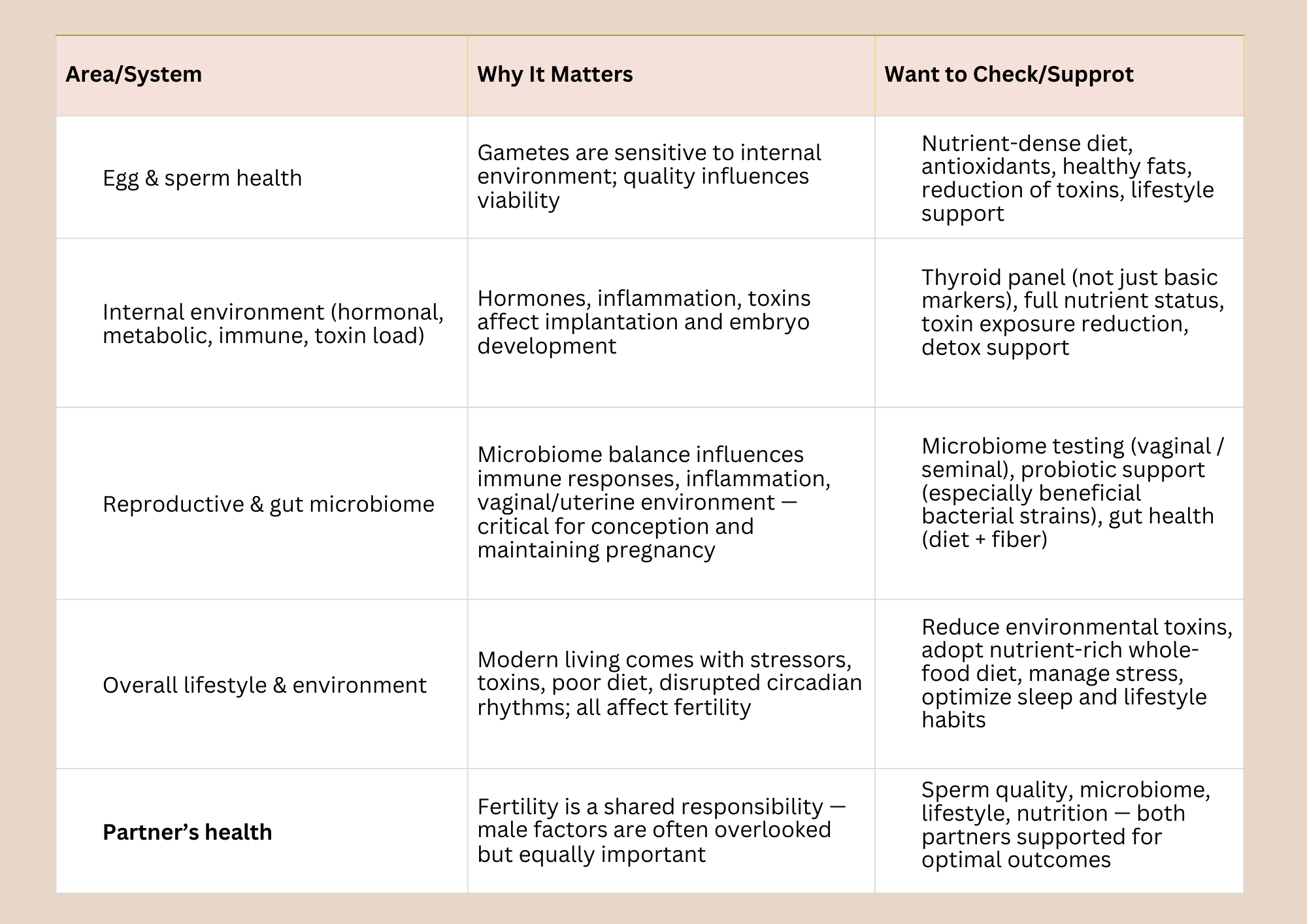
✔️ Key Areas to Investigate & Optimize for Fertility (Female & Male)
When supporting individuals/couples struggling with subfertility or recurrent miscarriage, a holistic practitioner may investigate and support across the following domains:
✔️ Nutritional & Lifestyle Foundations for Fertility
The guest recommends building fertility support around simple, sustainable, whole-food based, low-toxicity lifestyle changes, rather than radical or restrictive “diets.” Key principles:
Eat a rainbow of whole plant foods — lots of diverse vegetables, fruits, legumes, whole grains, nuts/seeds, healthy fats, lean proteins.
Focus on nutrient-dense, anti-inflammatory foods — high antioxidant load (colors = phytonutrients), healthy fats (omega-3), quality proteins, fiber.
Minimize/eliminate highly inflammatory foods: refined sugar, refined flours and oils, processed foods; for many, also reduce or eliminate gluten and dairy (common food triggers especially in subfertility / autoimmunity contexts).
Support gut & microbiome health: fiber, fermented foods or probiotics (particularly certain protective bacterial strains), support bowel regularity, avoid gut-irritating substances.
Optimize essential nutrients for fertility, hormone balance, and detoxification — e.g.: omega-3 fatty acids, B-vitamins (especially B12/folate/methylation support), magnesium, vitamin D (and K where relevant), antioxidants (vitamins A, E, etc.).
Use consistent small habits rather than drastic overhauls — small choices repeated over time yield cumulative benefit (e.g. adding herbs, a new vegetable, switching a product, reviewing environmental exposures).
✔️ The Microbiome: Not Just Gut — Reproductive Microbiome Matters
A newer and often overlooked piece: we are home to trillions of microbes not only in our gut, but also on skin, mouth, and — crucially for fertility — in the reproductive tract (vaginal/uterine in women; seminal tract in men).
A healthy reproductive microbiome (especially in females) tends to be dominated by protective bacteria (e.g. certain Lactobacillus species), which produce lactic acid and hydrogen peroxide — creating an environment that helps prevent pathogenic bacteria, supports implantation and healthy pregnancy.
Disruptions in this microbiome (history of thrush, BV, UTIs, hormonal imbalances, prior surgeries or interventions, or even repeated fertility treatments) can impair reproductive outcomes — even in absence of overt symptoms.
It’s not only women’s microbiomes: male partners’ semen microbiome also matters — beneficial microbes help support healthy sperm and a favorable environment for conception.
Testing is now accessible: there are at-home or practitioner-mediated vaginal microbiome and seminal microbiome test kits. For example:
InVivo Health — practitioner-mediated testing and female-probiotic products.
ScreenMe — consumer-accessible vaginal and seminal microbiome testing kits.
DAYE — test option especially useful for women with a history of HPV or abnormal smears.
If an imbalance is detected, interventions may include targeted probiotics or — in some cases — use of antibiotics (under clinical supervision), followed by microbial repopulation and support.
✔️ Importance of Thyroid & Hormones (Especially for Women Trying to Conceive)
Because almost every cell in the body has thyroid receptors, thyroid health directly affects energy metabolism, egg and sperm maturation, embryo development, and overall reproductive health.
Conventional thyroid testing (e.g. just TSH, basic Thyroxine) often misses subtler dysfunctions — and “normal” reference ranges may not be optimal for fertility. A more comprehensive thyroid panel is often more useful.
Low-functioning thyroid or autoimmune thyroid conditions can contribute to miscarriage, subfertility, hormonal imbalance, and poor pregnancy outcomes.
Supporting thyroid function through: balanced nutrition, sufficient antioxidants, liver/gut health, detoxification support, and reducing endocrine-disrupting toxins — all can make a meaningful difference.
✔️ Shared Responsibility: Male & Female Factors, Lifestyle & Environment
Fertility is rarely a “woman-only issue.” Male factors — sperm health, microbiome, lifestyle, toxin exposure — are equally critical and deserve attention.
Because sperm is regenerated every ~3–4 months, improvements in diet, lifestyle, and environment can — over time — lead to meaningful improvements in sperm quality.
Environmental toxins — plastics (e.g. BPA, phthalates), endocrine disruptors, pollutants, chemicals in personal care products — can interfere with hormonal balance, gamete quality, and reproductive outcomes.
Small, doable changes — replacing plastic containers with glass, switching to cleaner personal-care products, reducing exposure to harmful chemicals, improving air/food quality — over time collectively lower toxic load and support reproductive health.
✔️ What This Approach Offers: Hope, Control & a Compassionate Path Forward
Rather than accepting subfertility as a “fixed fate,” this integrative approach gives people agency, hope, and actionable steps — reducing feelings of helplessness, guilt, or despair.
It acknowledges the complexity of fertility — that many different systems (immune, hormonal, metabolic, microbiome, environmental) interact, and improvement often requires a multi-layered, personalized strategy.
It allows “normal life” to continue alongside efforts: changes don’t have to be extreme, prohibitive, or isolating. Small, consistent changes can be sustainable and empowering.
It encourages working in partnership — not just with one's medical provider, but as a couple (if applicable), prom
stay connected
One-to-One Nutritional Therapy
Hormone Insights & Support Service